Postpartum thyroid dysfunction is a common yet under-recognised condition that can significantly impact a new mother’s health. The physiological and hormonal changes of pregnancy and childbirth create a unique set of challenges for the thyroid gland. Understanding the common patterns seen postpartum and their underlying causes is essential for practitioners to provide effective support.
In this blog, we explore a detailed case study to illustrate the thyroid issues that can arise postpartum, along with practical strategies to address them.
The Case: Sarah’s Postpartum Journey
Background
Sarah, a 32-year-old first-time mother, presented at her six-month postpartum check-up with the following symptoms:
- Extreme fatigue, even after adequate sleep
- Difficulty losing weight despite a healthy diet and moderate exercise
- Increased sensitivity to cold
- Hair thinning and brittle nails
- Episodes of low mood and brain fog
- Breastfeeding her six-month-old baby
Sarah reported no significant medical history, but she did experience mild hypothyroid symptoms during her second trimester, which resolved without treatment. She had no family history of thyroid conditions but mentioned feeling particularly stressed and overwhelmed in the months following childbirth.
Assessment and Initial Observations
Clinical Presentation
- Puffy face and slight swelling around the neck, suggestive of thyroid enlargement.
- Dry skin and mild pallor.
Laboratory Tests Ordered
- Thyroid panel: TSH, free T4, free T3, reverse T3, and thyroid antibodies (TPO and Tg antibodies).
- Nutrient levels: Selenium, iodine, zinc, vitamin D, and iron.
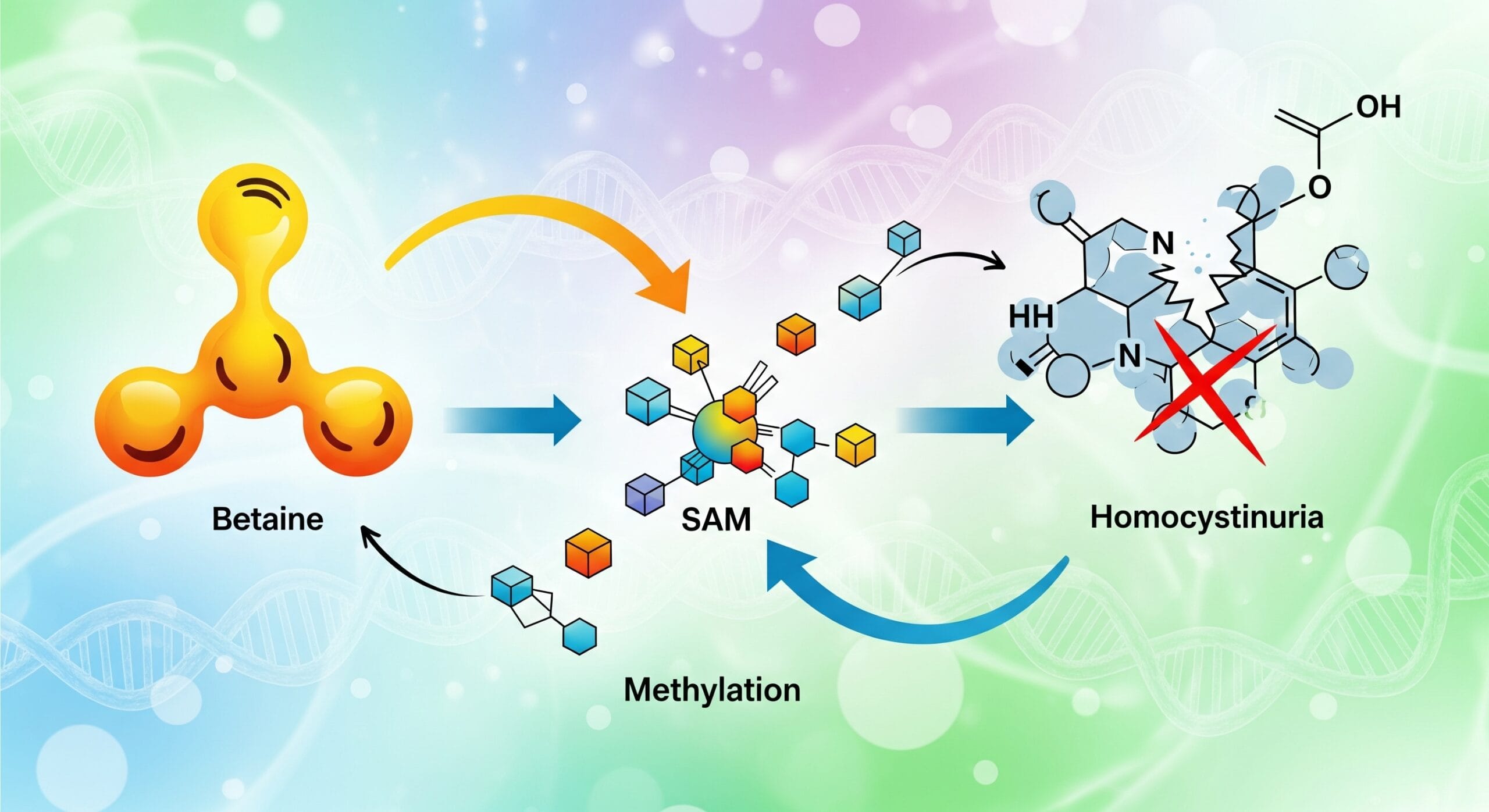
- Inflammation markers: CRP and homocysteine.
- Liver function: To assess T4 to T3 conversion capacity.
Results and Diagnosis
Lab Findings
- TSH: 4.8 mIU/L (high-normal)
- Free T4: 12 pmol/L (low-normal)
- Free T3: 3.2 pmol/L (low)
- Reverse T3: Elevated
- TPO antibodies: 150 IU/mL (elevated)
- Selenium: Low
- Iron: Ferritin at 10 µg/L (deficient)
- Vitamin D: 45 nmol/L (suboptimal)
- CRP: Elevated
Diagnosis
Sarah was diagnosed with postpartum thyroiditis, progressing into the hypothyroid phase, likely exacerbated by nutrient deficiencies, stress, and underlying inflammation.
Common Patterns in Postpartum Thyroid Dysfunction
Postpartum thyroid dysfunction often follows three stages:
- Euthyroid phase: Normal thyroid function in the early postpartum period.
- Hyperthyroid phase: Transient overactivity of the thyroid (increased T4 and T3) due to autoimmune activation, usually occurring 1-4 months postpartum.
- Hypothyroid phase: Depletion of thyroid reserves leading to low thyroid activity, often manifesting 4-8 months postpartum. This is the stage Sarah was experiencing.
The hypothyroid phase may resolve spontaneously, but in many cases, it can persist or evolve into chronic conditions like Hashimoto’s thyroiditis.
Key Contributing Factors
- Autoimmune Activation
- Pregnancy suppresses immune activity to protect the developing foetus. After delivery, immune activity rebounds, potentially triggering autoimmune conditions like Hashimoto’s or postpartum thyroiditis.
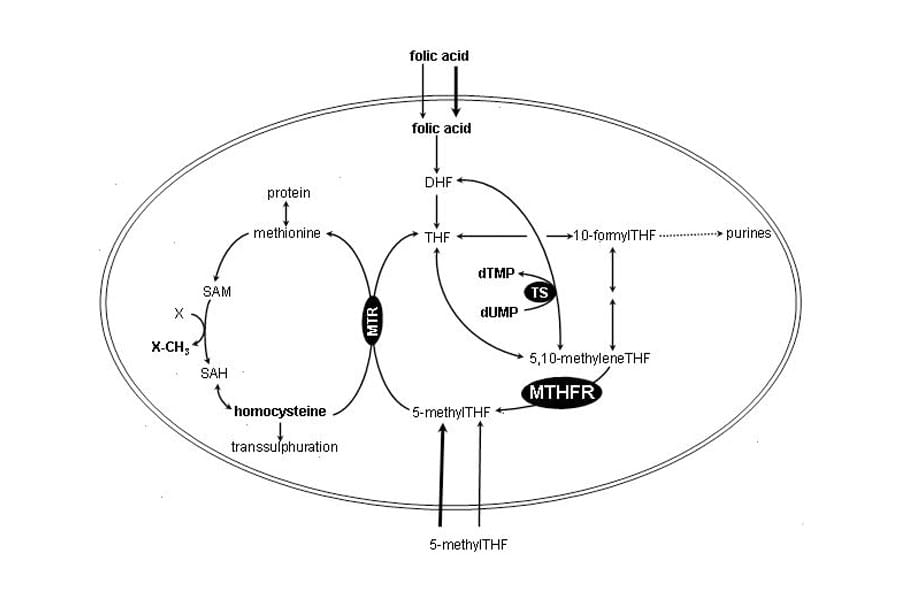
- Nutrient Depletion
- Pregnancy and breastfeeding deplete critical nutrients like iodine, selenium, iron, and zinc, all essential for thyroid hormone production and conversion.
- Stress and Inflammation
- Chronic stress elevates cortisol, increasing reverse T3 and impairing active T3 production. Inflammation exacerbates this process.
- Hormonal Shifts
- Dramatic changes in oestrogen and progesterone levels postpartum influence thyroid-binding globulin (TBG), affecting thyroid hormone availability.
Treatment Plan and Intervention
- Nutritional Support
- Iodine: 150 µg/day via kelp supplements to replenish stores.
- Selenium: 200 µg/day to support T4 to T3 conversion and reduce thyroid antibody levels.
- Iron: Iron bisglycinate (30 mg/day) with vitamin C to correct deficiency.
- Vitamin D: 2,000 IU/day to improve immune regulation.
- Stress Management
- Adaptogens: Ashwagandha to support the adrenal glands and reduce cortisol.
- Mindfulness and breathing exercises to mitigate stress-induced thyroid dysfunction.
- Dietary Recommendations
- A whole-food, anti-inflammatory diet with an emphasis on:
- Brazil nuts (selenium).
- Omega-3 fatty acids (salmon, flaxseeds).
- Dark leafy greens (iron and magnesium).
- Iodine-rich foods (seaweed, eggs).
- A whole-food, anti-inflammatory diet with an emphasis on:
- Thyroid Monitoring
- Regular thyroid panel testing every three months to monitor TSH, free T4, and free T3.
- Lifestyle Adjustments
- Encouraged light exercise such as walking or yoga to reduce stress and support overall metabolism.
Outcome
After three months of treatment, Sarah reported significant improvements:
- Energy levels normalised, and brain fog resolved.
- Hair loss reduced, and she began losing weight steadily.
- TSH levels decreased to 2.5 mIU/L, and free T3 improved to 4.1 pmol/L.
Her TPO antibodies also reduced to 70 IU/mL, indicating a decrease in autoimmune activity. Continued monitoring and support were recommended, with a focus on maintaining nutrient levels and managing stress.
Key Takeaways for Practitioners
- Test Thoroughly
Always include a full thyroid panel (TSH, free T4, free T3, reverse T3, and antibodies) and assess nutrient levels postpartum. - Address the Root Causes
Focus on reducing inflammation, repleting nutrients, and managing stress to support thyroid recovery. - Educate on Postpartum Risks
Many mothers are unaware of postpartum thyroid risks. Provide education about recognising symptoms early. - Personalise Treatment
Tailor interventions to each patient’s unique biochemical and lifestyle needs.